MACRA and MIPs
MACRA and MIPs
What is MACRA?
Simply put, MACRA is the new path to Medicare reimbursement.
MACRA, or the Medicare Access and CHIP Reauthorization Act, was signed into law on April 26, 2015. This law repeals the previously used Sustainable Growth Rate formula with a new program to pay physicians based on performance.
CMS (Centers for Medicare & Medicaid Services) has developed this program as part in a series of steps to prioritize care quality over volume. Starting in 2017, Medicare Part B providers enter a new payment framework called the Quality Payment Program (QPP).
What is QPP
- Quality Payment Program?
MACRA offers incredible financial opportunities for high-performance providers by associating reimbursements to value-based care.
CMS's Quality Payment Program (QPP) offers two new tracks to reimbursement: Merit-Based Incentive Payment System (MIPS)
and Advanced Alternative Payment Models (APMs).
What is MIPS?
MIPS, or the Merit-based Incentive Payment System, is a new payment track under Quality Payment Program where providers earn an adjustment on their Medicare payment based on performance. This track consolidates three existing programs (Meaningful Use, Physician Quality Reporting System and Value-Based Modifier) with the addition of a new component called Improvement Activities.
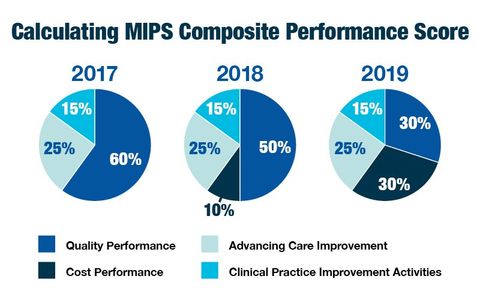
Providers earn the adjustment by showing they provided high quality, efficient care supported by technology by submitting information in four categories. The Cost category will be calculated in 2017, but will not be used to determine your payment adjustment. In 2018, CMS will start using the Cost category to determine the payment adjustment.
Who is Eligible?
Providers with 100 or more Medicare Part B patients, OR, more than $30,000 in Medicare allowables.
Check out CMS's Lookup Tool
to help clinicians determine their MIPS participation status for 2017.
Who Qualifies as an EP?
For 2017 and 2018: MDs, PAs, NPs, CNSs, CRNAs.
For 2019 and forward: PTs, OTs, SLs, Ps, AuDs, CNMs, LCSWs, LCPs, RDNs
Who is Exempted?
Qualifying APM (Alternative Payment Model) participants, providers with a minimum volume threshold of patients or payments, or providers in their first enrollment year with Medicare Part B.
How and when do I get started?
Providers can choose to start anytime between January 1 and October 2, 2017 however performance data must be submitted for at least a minimum of 90 days. Performance data must be submitted by March 31, 2018. The first payment adjustments based on performance go into effect on January 1, 2019.
CMS understands that 2017 is a transition year, so they have provided multiple participation levels so that providers can avoid penalties in 2019.
If you don’t send in any 2017 data, then you receive a
negative 4% payment adjustment.
If you submit a minimum amount of 2017 data (e.g. one
quality measure or one improvement activity), you can avoid a downward payment
adjustment.
If you submit 90 days of 2017 data, you may earn a neutral or small positive payment adjustment.
If you submit a full year of 2017 data, you may earn a moderate positive payment adjustment.
How will MIPS be scored?
Eligible clinicians (ECs) will be scored annually in the four performance categories to derive a MIPS composite score between 0 and 100. The four categories are Quality, Cost, Advancing Care Information and Improvement Activities. A clinician can choose to participate as an individual or in a group for each NPI/TIN combination that they bill under. CMS will apply the payment adjustment at the individual TIN/NPI level for all MIPS eligible clinicians.
You can count on us!
Our CaregiverDesktop EHR
solution is certified to meet
the ever-changing government healthcare requirements!